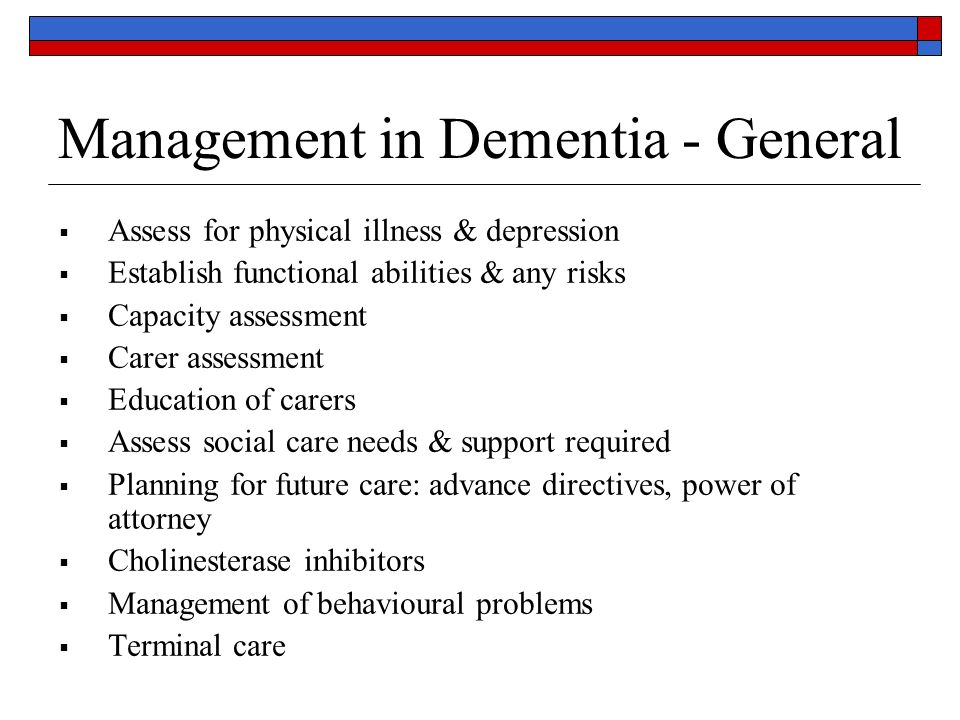
Strategies for improving behavior include ensuring that the patient's environment is safe, calm, and predictable; removing environmental stressors; and identifying and avoiding situations that agitate or frighten the patient. Simple interventions include redirecting and refocusing the patient, increasing social interaction, establishing regular sleep habits, eliminating sources of conflict and frustration, and establishing rewards for successes.
The effectiveness of long-term behavioral management is largely dependent on the caregiver; as such, it is important to assess the role and needs of the caregiver. Because currently available therapies cannot reverse the pathologic processes of AD, the primary objective of pharmacotherapy is to preserve cognitive and functional ability, minimize behavioral disturbances, and slow disease progression.
Cholinesterase inhibitors represent first-line therapy for patients with mild to moderate AD, whereas a glutamate N -methyl D -aspartate antagonist is used in the treatment of moderate to severe AD. Primary care is the point of first medical contact for people with dementia and hence the cornerstone of ensuring early detection, timely intervention, and effective ongoing management. Management consists of both pharmacologic and nonpharmacologic interventions as well as referrals to social service agencies and support resources, such as the Alzheimer's Association www.
The family physician plays a key role in linking the family to community resources and other health care and social service providers who will help implement the overall care plan. Moreover, the family physician can assist in maintaining the physical health of patients with dementia, for example, assisting with the evaluation and treatment of visual and hearing defects, which are more common with aging.
Such assistance can help directly and indirectly in the management of dementia. The primary research parameters were Alzheimer's disease , diagnosis , therapy , treatment , and therapeutic. Original research articles, reviews, and other articles of interest were reviewed, and the most important information was identified.
This review provides a summary of these findings as well as practical advice for the busy clinician.
Cleveland Clinic Menu
The management of a patient with AD is a complex and evolving task because the natural history of AD is one of progressive decline; patients' cognitive, physical, and social functions gradually deteriorate. In clinical trials, the Alzheimer's Disease Assessment Scale, Cognitive Subscale ADAS-Cog , a minute, item, point scale that tests memory, language, orientation, and praxis, is often used to determine rate of cognitive decline.
The total score ranges from 0 to 70, with a high score indicating greater impairment. In general, cholinesterase inhibitors ChEIs do not delay ultimate progression of AD by more than 6 to 7 months. An increasing number of nonpharmacologic therapies are now available for people with dementia, including behavioral therapy, reality orientation, art therapy, music therapy, complementary therapy, aromatherapy and bright-light therapy, as well as cognitive behavioral therapies.
There are several areas of overlap between these therapies and each approach is rarely used in isolation 14 ; it is therefore useful for clinicians to be familiar with several of these approaches to enable a combination of treatments to be tailored to individual requirements. Several nutrient deficiencies are known to be risk factors for AD. Evidence suggests that consumption of fish with high fat content and marine omega-3 polyunsaturated fatty acid decreases the risk of cognitive impairment and dementia.
However, to date, there are no clinical trials to support a recommendation of dietary and supplemental omega-3 polyunsaturated fatty acid for the sole purpose of preventing cognitive impairment or dementia. There has been recent attention regarding the health benefits of curcumin found in the commonly used Asian spice, turmeric in AD.
Finally, recent studies from both the United States and Europe have suggested that vitamin D deficiency may be associated with increased odds of cognitive impairment in older persons. Similar findings also have been reported in a European study. Medical foods as a class of intervention alternatives are not well known to most clinicians but are a growing area.
Medical foods are a special category of US Food and Drug Administration FDA —regulated agents intended to provide specific nutritional requirements for patients with certain diseases; they can, therefore, provide an additional supplement in a comprehensive therapeutic regimen for patients with AD. Products being marketed currently or developed in the United States for the management of dementia include Caprylic triglyceride Axona, Accera, Inc.
Axona has been developed for the clinical dietary management of the metabolic processes associated with mild to moderate AD. Souvenaid food combines omega-3 fatty acids, choline, uridine monophosphate, and a mixture of antioxidants and B vitamins. There are currently no means of reversing the pathologic processes of AD. Currently available medications do not halt the underlying degenerative process but can slow disease progression and therefore delay symptomatic decline.
The main benefit of pharmacotherapy is an attenuation of decline over time rather than an improvement in cognitive or behavioral symptoms. It is important to discuss this point with patients and their families, who may expect improvement rather than relative stability. Beneficial response to a ChEI ie, delayed deterioration of cognitive or behavioral problems can be determined from the physician's global assessment of the patient, the primary caregiver's report, a neuropsychologic assessment or mental status questionnaire, or evidence of behavioral or functional changes.
Four drugs are commonly used for treating AD: Since the introduction of the first ChEI in , most clinicians would consider these agents to be first-line pharmacotherapy for mild to moderate AD. Tacrine is not commonly used because of a poor tolerability profile and low oral bioavailability, and it is, therefore, excluded from this discussion. However, the cm 2 rivastigmine patch has shown efficacy similar to oral rivastigmine formulations, but with approximately two-thirds fewer reports of nausea and vomiting, with adverse event AE rates similar to those of placebo 32 Table 1.
- Redemption?
- Dementia - Diagnosis and treatment - Mayo Clinic;
- E003: FREUNDINNEN (eBook Erotik) (German Edition).
- AGING, DEPRESSION AND DEMENTIA;
- INTRODUCTION;
- Dementia diagnosis?
- Guidelines for the Management of Cognitive and Behavioral Problems in Dementia.
There continues to be debate regarding the extent of the benefits achieved with ChEIs. Although some assert that the most that can be achieved with ChEIs is symptom modification, 11 others consider these agents to have disease-modifying effects. A systematic analysis of double-blind, placebo-controlled trials of ChEIs demonstrated treatment effects ranging from a 1. In addition to their effects on cognition, these agents also have demonstrated beneficial effects on measures of behavior, activities of daily living ADLs , and global patient function.
A recent meta-analysis that analyzed clinical results from 29 randomized, placebo-controlled trials of patients with mild to moderate AD found that ChEI therapy was associated with significant modest benefits in terms of neuropsychiatric and functional outcomes. ChEIs also have been shown to reduce AD caregiver burden: Memantine Namenda, Forest Pharmaceuticals, St.
Although memantine has been reported to improve cognition, global status, and behavior in patients with mild to moderate AD, 48 its mechanism of action would suggest that it does not have a place in early AD. Memantine is not a ChEI; it is a low- to moderate-affinity, noncompetitive channel blocking , NMDA-receptor antagonist that seems to block pathologic neural toxicity associated with prolonged glutamate release.
Memantine is approved for the treatment of moderate to severe AD on the basis of a study in which patients with moderate to severe AD who received 20 mg memantine monotherapy showed less decline in cognition and function while maintaining good tolerability after 6 months compared with those who received placebo. Combination therapy of a ChEI and memantine is rational from a pharmacologic perspective because the agents have different mechanisms of action. In a randomized controlled trial, patients with moderate to severe AD who were already receiving donepezil derived significant benefit from the addition of memantine in terms of cognition, ADLs, global outcome, and behavior.
A recent study demonstrated improvement in clinical outcomes plus cost savings associated with the use of memantine. The safety and tolerability of combining rivastigmine capsule and memantine also has been studied in a week, prospective, open-label study of patients with moderate AD. A recent study has demonstrated that ChEI-treated patients with early AD who received psychosocial support plus cognitive-motor intervention CMI had additional mood and cognitive benefits over those experienced by ChEI-treated patients who received psychosocial support alone.
The CMI consisted of a 1-year structured program of sessions, including reality orientation techniques, cognitive exercises, training of ADLs, and psychomotor exercises. The ADL training was related to the particular cognitive function stimulated at each session eg, money handling was trained after calculation exercises. The results showed that patients in the CMI group maintained cognitive status at 6 months, whereas patients in the control group had significantly declined by that time.
In , a panel of leading experts published recommendations for best practice in the treatment and management of AD. These recommendations were developed in an effort to address issues surrounding early diagnosis, treatment, and care management of AD, as well as societal and managed-care implications. Alternatively, global guidelines recommend that patients who continue on the drug should be reviewed every 6 months by MMSE score and global, functional, and behavioral assessment. Treatment and management of Alzheimer disease. This treatment algorithm is derived from recommendations published in Ref.
Reproduced with permission from RG Stefanacci. Reinforcing the value of combination therapy to treat moderate to severe alzheimer's disease. Phys Week ;26 9. Traditionally, cognitive function has been the main focus of interest in treatment and research of people with dementia. It is becoming increasingly recognized, however, that noncognitive symptoms are those that are most disturbing to families and caregivers and may seriously impact not only the patient's well-being, but also the family's, caregivers', and providers' approaches to managing the patient.
Furthermore, environmental factors eg, confusing or noisy surroundings or interpersonal factors eg, arguing with the patient are often the primary triggers of behavior problems. Attention to these factors through nonpharmacologic approaches can be effective in alleviating or preventing behavioral problems in individuals with dementia and should be considered first.
Unfortunately, in practice, pharmacologic approaches involving neuroleptic or other sedative medication are often used as the first-line treatment, despite the modest evidence of efficacy from clinical trials in which high placebo response rates frequently are seen. Patients with AD function best in an environment that is safe, calm, and predictable, and their caregivers require ongoing support and education to develop realistic expectations throughout the course of the illness.
A predictable routine also is important and may avert certain behavioral problems. For example, scheduled toileting or prompted voiding can reduce urinary incontinence. Nonpharmacologic interventions can be as simple as redirecting and refocusing the patient, increasing social interaction, initiating enjoyable activities, establishing regular sleep habits, eliminating sources of conflict and frustration eg, activities that the patient can no longer undertake , and establishing rewards for successes, however small Table 2.
Patients of certain faiths may become agitated during intimate situations, such as bathing or dressing, when in the presence of caregivers who are of the opposite sex; a caregiver of the same sex may lead to improvement in behavior. The removal of any triggers of behavioral problems or the provision of comforting stimulation, such as the patient's favorite music, also may be beneficial. The use of behavioral interventions in dementia is hindered by the fact that the patient's cognitive functioning is declining progressively.
As such, the effects of interventions must be monitored continually and adjustments made over time in response to new behaviors that may emerge. Over the past 10 years there has been an increasing interest in applying therapeutic frameworks, such as cognitive behavioral therapy CBT , cognitive stimulation therapy CST , and interpersonal therapy to dementia.
- Guitar Method: Winter in Seattle;
- The Hunt for the Well Hidden Treasure (K.I.D.S. Adventure Series Book 1).
- Conscious Capitalism, With a New Preface by the Authors: Liberating the Heroic Spirit of Business!
- Clinical Practice Guidelines for Management of Dementia!
- The Family of God & The New Birth.
- Time, Change, and the American Newspaper (Routledge Communication Series)!
These therapies are designed to actively stimulate and engage people with dementia; group therapy, such as that used for CST, provides an optimal learning environment and the social benefits of a group and aims to create an environment in which people learn and strengthen their existing resources. The principles of person-centered care are essential when delivering CST for individuals with dementia; as such, group members often are assigned a role within the group according to their interests and abilities.
During each themed session, there is a range of activities available, which allows the facilitator to adapt the level of difficulty of the activities depending on the group's cognitive capabilities, interests, and gender mix; each individual can be provided with an activity suitable for him or her personally.
Individuals are asked to give their opinions rather than provide factual answers, and multisensory stimulation is used when possible. Teri and Gallagher-Thompson 71 reported positive findings from a clinical trial of CBT with individuals with early AD, and individual and group CBT also has been used with some favorable results. Put simply, many of the challenges posed by people with dementia are caused by their thinking style—the very thing that is addressed in CBT.
CBT, therefore, offers a framework within which to understand the individual's distressing experiences, and this understanding allows the clinician to target interventions more appropriately. Pharmacologic interventions are necessary when nonpharmacologic strategies fail to reduce behavioral symptoms sufficiently. If behavioral disturbances persist despite the use of ChEIs, memantine, or both, a psychotropic agent may be necessary.
After behavioral disturbances have been controlled for 4 to 6 months, the dosage of the psychotropic agent can be reduced periodically to determine whether continued pharmacotherapy is required.
Coping with dementia
The choice of psychopharmacologic agent is determined by specific target symptoms; some behaviors, such as wandering and pacing, are not amenable to drug therapy. Medications used to treat behavioral disturbances and mood disorders are summarized in Table 3. Atypical antipsychotic drugs have been commonly used off-label in clinical practice for treatment of serious, dementia-associated agitation and aggression, although they are not approved by the FDA for such use. In addition, these agents have a black-box warning of increased mortality among elderly patients with dementia-related psychosis.
A meta-analysis assessed the evidence for increased mortality from atypical antipsychotic drug treatment for people with dementia. A total of patients were randomized to study drug and were randomized to placebo. They concluded that problems in clinical trial design may have contributed to the negative results reported and suggested that future studies be required to address the benefit—risk balance in this patient population. If antipsychotics are indicated, then it is recommended that they are used at the lowest effective dose, with dosage reduced or treatment discontinuation considered on a regular basis.
Agitation and psychosis are distressing and are likely to overwhelm the caregiver's ability to cope. If behavioral and nonpharmacologic interventions are inadequate, mild agitation can be managed with low doses of medications, such as trazodone, carbamazepine, and valproate. Studies have demonstrated benefits for agitation with citalopram compared with placebo 76 and similar efficacy compared with risperidone. Apathy as a distinct psychiatric syndrome is an evolving concept but generally has been defined as poor initiation, impaired persistence, indifference, reduced emotional response, and low social engagement.
Depression is common in older adults, including those with AD, and often is undiagnosed and untreated. The efficacy of antidepressants in patients with AD who also suffer depression has been demonstrated in clinical trial; the most useful medications are those with minimal anticholinergic side effects. Selective serotonin reuptake inhibitors, such as citalopram Celexa, Forest Laboratories, Inc.
Caregivers can become exhausted and frustrated; suffer depression, anxiety, and health problems; and be at increased risk of death. One study has reported that the most consistently effective method of caregiver treatment interventions is to teach caregivers how to change or modify their interaction with the patient. Mittelman and colleagues 82 have demonstrated the effectiveness of long-term behavioral interventions for caregivers. Caregivers of patients with AD often suffer from depression, and optimizing long-term social support individual and family counseling, the continuous availability of ad hoc counseling, and support group participation can have a significant impact on depression in caregivers.
In the event that insufficient resources are available to provide for and protect both patient and caregiver, nursing home placement needs to be considered. Although consideration of the patient's previously expressed wishes is essential, caregivers often feel constrained by comments made years earlier and believe that the patient would not accept long-term care.
It can be helpful to remind caregivers that earlier comments were made without a full appreciation of the current circumstances and that expectations almost always change with chronic illnesses. ChEIs and memantine are symptomatic therapies that help maintain neuronal function but do not have a significant impact on the underlying disease process. Their benefits are mild, and treatments that modify the disease course are urgently needed.
There recently has been intense research interest in characterizing the earliest stages of AD that precede the crossing of the dementia threshold, defined by functional disability. AD currently is thought to be a complex, multifactorial syndrome, unlikely to arise from a single causal factor; instead, a number of related biologic alterations are thought to contribute to its pathogenesis.
In light of this, drug combinations that can act at different levels of the neurotoxic cascade offer new avenues toward curing AD and other neurodegenerative diseases. Family physicians play a crucial role in the care of patients with AD in terms of early detection, timely intervention, and effective ongoing management. Optimal management involves a multidimensional approach to treatment that includes the physician, geriatric care managers, social services, and the patient's family.
The treatment of AD consists of both pharmacologic and nonpharmacologic interventions. Nonpharmacologic interventions are recommended as the most appropriate initial strategy for managing problematic behaviors. Patients with AD function best in an environment that is safe, calm, and predictable. Interventions for improving behavior include reduction of environmental stressors and strategies to reduce the agitation and anxiety of the patient.
These interventions can be as simple as redirecting and refocusing the patient, increasing social interaction, establishing regular sleep habits, eliminating sources of conflict and frustration, and establishing rewards for successes, however small. The role and needs of the caregiver are important, and the effectiveness of long-term behavioral interventions for caregivers has been demonstrated.
In the absence of means to reverse the pathologic processes of AD, the primary objectives of pharmacologic interventions are to preserve cognitive and functional ability, minimize behavioral disturbances, and slow disease progression. At present, four drugs are widely used to treat AD: The authors would like to thank Frances Gambling for her editorial assistance with the manuscript. Administrative, editorial, and technical assistance was funded by Novartis Pharmaceuticals Corporation. CHS has served as a consultant to Novartis Pharmaceuticals Corporation; has served as a speaker for Novartis Pharmaceuticals Corporation, Forest Pharmaceuticals, and Accera; and has received honoraria from both companies.
Neither author received financial support for this manuscript. Sadowsky , MD and James E. Previous Section Next Section. Goals of Therapy and Likely Outcomes The management of a patient with AD is a complex and evolving task because the natural history of AD is one of progressive decline; patients' cognitive, physical, and social functions gradually deteriorate. Nonpharmacologic Interventions An increasing number of nonpharmacologic therapies are now available for people with dementia, including behavioral therapy, reality orientation, art therapy, music therapy, complementary therapy, aromatherapy and bright-light therapy, as well as cognitive behavioral therapies.
Medical Foods Medical foods as a class of intervention alternatives are not well known to most clinicians but are a growing area. Pharmacologic Interventions There are currently no means of reversing the pathologic processes of AD. In this window In a new window. Mild to Moderate Disease Since the introduction of the first ChEI in , most clinicians would consider these agents to be first-line pharmacotherapy for mild to moderate AD.
Moderate to Severe Disease Memantine is approved for the treatment of moderate to severe AD on the basis of a study in which patients with moderate to severe AD who received 20 mg memantine monotherapy showed less decline in cognition and function while maintaining good tolerability after 6 months compared with those who received placebo. Adjuncts to Pharmacotherapy for Improving Cognitive Function A recent study has demonstrated that ChEI-treated patients with early AD who received psychosocial support plus cognitive-motor intervention CMI had additional mood and cognitive benefits over those experienced by ChEI-treated patients who received psychosocial support alone.
Treatment Guidelines In , a panel of leading experts published recommendations for best practice in the treatment and management of AD. Cognitive Behavioral Therapy Over the past 10 years there has been an increasing interest in applying therapeutic frameworks, such as cognitive behavioral therapy CBT , cognitive stimulation therapy CST , and interpersonal therapy to dementia.
Pharmacologic Interventions Pharmacologic interventions are necessary when nonpharmacologic strategies fail to reduce behavioral symptoms sufficiently. Pharmacologic Treatment of Behavior and Mood Disorders. Atypical Antipsychotics Atypical antipsychotic drugs have been commonly used off-label in clinical practice for treatment of serious, dementia-associated agitation and aggression, although they are not approved by the FDA for such use.
Agitation Agitation and psychosis are distressing and are likely to overwhelm the caregiver's ability to cope. Apathy Apathy as a distinct psychiatric syndrome is an evolving concept but generally has been defined as poor initiation, impaired persistence, indifference, reduced emotional response, and low social engagement. Depression Depression is common in older adults, including those with AD, and often is undiagnosed and untreated. Effectiveness of educational interventions in improving detection and management of dementia in primary care: BMJ ; General practitioners on dementia: Patient Educ Couns ; CrossRef Medline Google Scholar.
Patterns of care in the early stages of Alzheimer's disease: J Am Geriatr Soc ; New drugs for Alzheimer's disease and other dementias. Br J Psychiatry ; STEP 3 Evaluation after recognition of the syndrome of dementia look for medical problems. Cognitive assessment can be made as part of detailed examination of higher functions. Addenbrooke's Cognitive Examination ACE is a more detailed test battery for assessing cognitive functions.
Assessment of the activities of daily living is very important. This information is essential in formulating the individualized plan of intervention. Use of simple instruments like the Clinical Dementia Rating Scale can help in assessing the severity of dementia in routine clinical practice. Assessment of non-cognitive symptoms like Behavioural and Psychological Symptoms of Dementia BPSD is yet another important part of clinical assessment. ICD- 10 clinical criteria may be used for diagnosis of Dementia and subtyping.
Alterantively one could use the DSM-5 criteria too. You may use the consensus clinical diagnostic criteria. After detailed assessment usually, the clinician would be in a position to judge the cause of the dementing illness. Clinical recognition of the subtypes of dementia is important and is easier during the early part of the illness. Such differentiation is feasible in clinical practice by using clinical criteria for these subtypes. The clinicians might choose any standard criteria for making clinical diagnosis of dementia, especially common sub-types.
See Table 6 for the criteria which may be useful in clinical practice. The impairment applies to both verbal and non-verbal material. The decline should be objectively verified by obtaining a reliable history from an informant, supplemented, if possible, by neuropsychological tests or quantified cognitive assessments.
Dementia: assessment, management and support: summary of updated NICE guidance
The severity of the decline, with mild impairment as the threshold for diagnosis, should be assessed as follows:. The main function affected is the learning of new material. For example, the individual has difficulty in registering, storing and recalling elements in daily living, such as where belongings have been put, social arrangements, or information recently imparted by family members.
A degree of memory loss which represents a serious handicap to independent living. Only highly learned or very familiar material is retained. New information is retained only occasionally and very briefly. The individual is unable to recall basic information about where he lives, what he has recently been doing, or the names of familiar persons.
Only fragments of previously learned information remain. The subject fails to recognize even close relatives. Evidence for this should be obtained when possible from interviewing an informant, supplemented, if possible, by neuropsychological tests or quantified objective assessments. Deterioration from a previously higher level of performance should be established.
The decline in cognitive abilities causes impaired performance in daily living, but not to a degree making the individual dependent on others. More complicated daily tasks or recreational activities cannot be undertaken. The decline in cognitive abilities makes the individual unable to function without the assistance of another in daily living, including shopping and handling money. Within the home, only simple chores are preserved. Activities are increasingly restricted and poorly sustained. The decline is characterized by an absence, or virtual absence, of intelligible ideation.
The overall severity of the dementia is best expressed as the level of decline in memory or other cognitiveabilities, whichever is the more severe e. Preserved awarenenss of the environment i. When there are superimposed episodes of delirium the diagnosis of dementia should be deferred. A decline in emotional control or motivation, or a change in social behaviour, manifest as at least one of the following:.
For a confident clinical diagnosis, G1 should have been present for at least six months; if the period since the manifest onset is shorter, the diagnosis can only be tentative. The diagnosis is further supported by evidence of damage to other higher cortical functions, such as aphasia, agnosia, apraxia. Judgment about independent living or the development of dependence upon others need to take account of the cultural expectation and context. Dementia is specified here as having a minimum duration of six months to avoid confusion with reversible states with identical behavioural syndromes, such as traumatic subdural haemorrhage S The diagnosis is confirmed by post mortem evidence of neurofibrillary tangles and neuritic plaques in excess of those found in normal ageing of the brain.
The following features support the diagnosis, but are not necessary elements: Involvement of cortical functions as evidenced by aphasia, agnosia or apraxia; decrease of motivation and drive, leading to apathy and lack of spontaneity; irritability and disinhibition of social behaviour; evidence from special investigations that there is cerebral atrophy, particularly if this can be shown to be increasing over time.
In severe cases there may be Parkinson-like extrapyramidal changes, logoclonia, and epileptic fits. Specification of features for possible subtypes. Because of the possibility that subtypes exist, it is recommended that the following characteristics be ascertained as a basis for a further classification: The division of AD into subtypes can at present be accomplished in two ways: Revised criteria for the clinical diagnosis of probable and possible dementia with Lewy bodies DLB.
DLB should be diagnosed when dementia occurs before or concurrently with parkinsonism. The term Parkinson disease dementia PDD should be used to describe dementia that occurs in the context of well-established Parkinson disease. In a practice setting the term that is most appropriate to the clinical situation should be used and generic terms such as Lewy body disease are often helpful. In research studies in which distinction needs to be made between DLB and PDD, the existing 1-year rule between the onset of dementia and parkinsonism continues to be recommended.
Multimorbidity is common in latelife. A clear understanding of physical aand mental health is important for planning dementia care. Please see table 7 for follow up plans. Non-pharmacological management strategies Table -8 have an important role in the management of dementia of any type. It is particularly helpful in elderly patients who may not tolerate pharmacological agents due to the development of adverse effects even in smaller doses. There are specific non-pharmacological interventions targeting the cognitive as well as non-cognitive symptoms and challenging behaviours seen in dementia.
Pharmacological treatment for Behavioural and Psychological symptoms of dementia Table The course of Dementia can be divided into three phases; mild, moderate and severe, based on the severity of cognitive symptoms and functional impirment. BPSD may not be present in all cases and may not be problematic in some. Mangement of BPSD is particularly important during the initial phases of the illness as this can have direct impact on the quality of life of the affected individual and the family members involved in care.
Refer to the setion on management. Older people with dementia have high risk of development delirium. Both hypoactive and hyperactive delirium can occur, but hypoactive delirium is more likely. Any sudden deterioration in sensorium, activity level, behaviour should alert the possibility of superimposed delirium. It will be be associated with disturbance in sleep wake cycle and could also take the form of increased sleepiness. The management should involve attempts to identify multiple causes which usually contribute to development and persistence of delirium.
Once identified these factors may be addressed and the condition be monitored. Disappearance of recent onset behavioural symptoms and improvement in cognitive functions over a period of days would usually be indicative of resolution of superimposed delirium. Dementia is a major neuropsychiatric condition and long-term medical care. Multimorbidity is common among older people and people with dementia are no exception. Two strategies can help here. The first one is to evaluate the person in detail for presence of co-morbidity and sensory impairments.
This can be done after making the diagnosis of dementia. Do enquire about the current management of each problem. You may include the management of the co-morbid conditions also into the follow-up plan. The second important strategy would be to be on the watch out for emergence of new problems like delirium or issues related falls, infections, cerebrovascular events etc. Prompt identification and early interventions can help to prevent or identify major eventsearly. Adherence to interventions is a matter of concern as this would be dependent on the caregivers.
Communication with the caregivers will have to be simple and might need to be repeated. Try to speak to the primary caregivers directly and allow time for clarifications if they have doubts. Ask a family member to take up the responsibility of co-ordinating and monitoring home-based care and to report the progress during follow up visit.
The primary caregiver is the ideal person to do this. But resource limitations are frequent and providing more caregiver support during trying times can be a great help for families involved in dementia care. Judicious modification of the home environment will help. An informed caregiver can discuss this and do the needful.
Discussions with caregivers and other family members will allow innovations which will may suit the particular home setting. All falls increase the risk of fractures and a fracture hip can have a very negative outcome for an older person with dementia. Need to Link with Community-based ServicesIt would help if community outreach services like palliative care services or any other similar service can be linked to home-based dementia care.
Brief screening tests can be useful. This can help in eliciting key information and by making brief cognitive assessment. The ideal test would be sensitive and specific. It should be short, simple and user friendly. There are large number of tests available and that suggests that no one test is the best.
Shorter tests may confirm a cognitive problem that needs to be evaluated, whereas longer tests contribute more to the diagnosis.
There are many instruments useful to screen or find cases of dementia. Details of useful tools are available at the website of Alzheimer's Association https: Caregiver support and non-pharmacological interventions to manage symptoms like BPSD are the main ingredients of dementia care. Psychosocial management forms the first line and shall be given to all with BPSD. Psychosocial interventions work best when it is contextualized to the socio-cultural environment and the setting of care.
Family and professional caregivers should be considered as key collaborators. Provision of relevant information, education and seamless support to caregivers, will be very crucial in dementia care. There is unmet need for such help and guidance. The families engaged in the care of a person affected by dementia will benefit from such support and this is especially so there are behavioral symptoms which are difficult to mange in home setting Some may benefit from pharmacological interventions but this shall be provided under supervision and needs to be monitored.
National Center for Biotechnology Information , U. Journal List Indian J Psychiatry v. Sivakumar , 1 G. Prasad Rao , 2 and Neelanjana Paul 3. Neelanjana Paul 3 Department of Psychiatry, moc. The disabilities progress with the severity of dementia Cognitive changes that are part of normal aging process has to be differentiated from the dementia syndrome. Propensity to develop transient cognitive problems like delirium increases with age and in the presence of cognitive impairment Evaluation of cognitive symptoms Cognitive symptoms can be due to many conditions and dementia is only one of them.
Table 1 Assessment for dementia. Open in a separate window. History of Cognitive Changes History taking is the main tool in eliciting and evaluating the nature and progression of cognitive decline. Importance of Identification of Delirium Delirium is an important differential diagnosis of dementia. Objective evidence from history, physical and neurological examination or laboratory tests of an underlying cerebral or systemic disease other than psychoactive substance-related that can be presumed to be responsible for the clinical manifestations in A-D.
Common causes of Delirium include:. Drugs particularly those with anticholinergic side effects e. Dementia with Psychotic Symptoms and Schizophrenia Presence of BPSD, especially delusions with or without hallucinations in mild to moderate dementia can resemble schizophrenia or other psychotic conditions in late life. See table-3 for some clinical tips Table 3 Psychosis of AD compared with Schizophrenia in the elderly.
Evidence of modest cognitive decline from a previous level of performance in one or more cognitive domains complex attention, executive function, learning and memory, language, perceptual motor, or social cognition based on:. Concern of the individual, a knowledgeable informant, or the clinician that there has been a mild decline in cognitive function; and. A modest impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment.
The cognitive deficits do not interfere with capacity for independence in everyday activities i. The cognitive deficits are not better explained by another mental disorder e. Assessment of Dementia Syndrome We need to rule out delirium and mild cognitive disorder before we make a clnical diagnosis of dementia.
Types and Causes of Dementia Dementia is a syndrome which can be caused by many diseases. Clinical Assessment Patients who seek help in clinical settings often do not represent cases prevalent in the community. Common Potentially Reversible Causes Depression. Table 5 Common Subtypes of Irreversible Dementias. Table 6 Diagnostic criteria for Dementia. Evidence of each of the following: The severity of the decline, with mild impairment as the threshold for diagnosis, should be assessed as follows: A decline in emotional control or motivation, or a change in social behaviour, manifest as at least one of the following: There is no evidence from the history, physical examination or special investigations for any other possible cause of dementia e.
B12 or folic acid deficiency, hypercalcaemia , or alcohol- or drug-abuse. The general criteria for dementia G1 to G4 must be met. Unequal distribution of deficits in higher cognitive functions, with some affected and others relatively spared. Thus memory may be quite markedly affected while thinking, reasoning and information processing may show only mild decline. There is clinical evidence of focal brain damage, manifest as at least one of the following:. There is evidence from the history, examination, or tests, of a significant cerebrovascular disease, which may reasonably be judged to be etiologically related to the dementia e.
Insidious onset and gradual progression. Decline in personal hygiene and grooming. Essential for a diagnosis of DLB is dementia, defined as a progressive cognitive decline of sufficient magnitude to interfere with normal social or occupational functions, or with usual daily activities. Prominent or persistent memory impairment may not necessarily occur in the early stages but is usually evident with progression.
Deficits on tests of attention, executive function, and visuoperceptual ability may be especially prominent and occur early. Core clinical features The first 3 typically occur early and may persist throughout the course. Fluctuating cognition with pronounced variations in attention and alertness.
One or more spontaneous cardinal features of parkinsonism: Severe sensitivity to antipsychotic agents postural instability; repeated falls; syncope or other transient episodes of unresponsiveness; severe autonomic dysfunction, e.
Abnormal low uptake iodine-MIBG myocardial scintigraphy. Polysomnographic confirmation of REM sleep without atonia. Two or more core clinical features of DLB are present, with or without the presence of indicative biomarkers. Only one core clinical feature of DLB is present, with no indicative biomarker evidence. In the presence of any other physical illness or brain disorder including cerebrovascular disease, sufficient to account in part or in total for the clinical picture, although these do not exclude a DLB diagnosis and may serve to indicate mixed or multiple pathologies contributing to the clinical presentation.
I parkinsonian features are the only core clinical feature and appear for the first time at a stage of severe dementia. This is essentiality about the the ablity for feeding, bathing, dressing, mobility, toileting, continence and also the ability to manage finances and medications. Poor nutritional status can be a consequence of poor self care and poor dietary intake.
Identify the Primary caregiver. In most instances there will be one person who generally co-ordinates and provide most of the care provision. Please follow the earlier described format to make assessments when there is history of cognitive decline. Those steps will help to identify and differentiate between syndromes like delirium, dementia and mild cognitive disorder.
Once the dementia syndrome is identified the assessments shall be aimed at the following. By and large the commonest setting for dementia care. The need is to identify and support the needs of home-based care.
Dementia: assessment, management and support: summary of updated NICE guidance | The BMJ
They may contact local chapters of Alzhiemer's and Related Disorders Society, Help Age India, Paliative Care Networks, other voluntary agencies engaged in geriatric care and seek support and guidance. When the hom-based care is not feasible or unavailable, the person with dementia may need instituitional care with provision for assisted living. This is often required when there is a medical or surgical morbidity which often cannot be handled in ambulatory care settings. Onset of delirium or sudden worsening of BPSD also could necessitate brief hospitalization.
Brief hospitalisations can be used to provide more information and assistance to caregivers. This can be an opportunity to identify unmet care needs as well as needs of the caregivers. There is a need for this facility especially when the home-based care is not able to meet the demands of care.
This is a reality in many household as the family size is dwindling and most young people work outside their homes. People with mild to moderate dementia of all types should be encouraged to participate in structured cognitive stimulation programmes. They benefit cognition in such patients irrespective of whether any drug is prescribed or not. They are also beneficial in improving and maintaining their functional capacity. This is based on the view that lack of cognitive activity hastens cognitive decline. Reality orientation and reminiscence therapy is of use in this regard.
Non-pharmacological interventions for non-cognitive symptoms and challenging behaviour. Non-cognitive symptoms and challenging behaviors significantly increase the burden of care. They lead to caregiver distress and burnout and hence is an important concern in the management of dementia. Common non-cognitive symptoms seen in dementia are delusions, hallucinations, anxiety, agitation and associated aggressive behavior. Challenging behaviours include a range of difficulties experienced by people with dementia and has a considerable impact on their caregivers.
Common challenging behaviours are aggression, agitation, wandering, hoarding, sexual disinhibition, apathy and shouting. Non-pharmacological interventions for the non-cognitive symptoms and challenging behaviours should be tailored for each patient with participation from the caregivers. This shall be preceded by assessments aimed at identifying factors which may be responsible to generate, aggravate or improve such behaviour. Such an assessment should be comprehensive and consider the person's physical health, possible undetected pain or discomfort, side effects of medication, psychosocial factors, cultural and religious background, and physical environmental factors.
The choice of therapy should be made considering the availability along with the person's preferences, skills and abilities. These interventions can be delivered by health and social care staff and volunteers with proper training and supervision.
